Governor Asa Hutchinson announced on Wednesday, June 17, that Arkansas will allow visitation at some long-term care facilities to resume effective July 1. The Arkansas Department of Health released the following guidelines:
A nursing home, assisted living facility, or residential care facility may expand visitation and other activities covered by the directive issued by the Arkansas Department of Health on March 13, 2020, only as provided by this directive. To be eligible to expand visitation and other activities, a facility must meet the following facility-specific requirements:
Facility-specific Requirements
• The facility has completed baseline testing of all residents and staff at least once and has provided the results and all requested documentation of such to the Arkansas Department of Health. • The facility has complied with these requirements and all other guidelines issued by the Arkansas Department of Health after baseline testing in response to any positive cases identified during baseline testing. • There are adequate hospital beds and ICU services available in the applicable region to serve any new COVID-19 cases, as determined by the Arkansas Department of Health. • The facility is able to staff direct care, housekeeping, and dietary services departments to meet the needs of the residents and existing legal requirements. • The facility has proper PPE and sufficient supply for residents and staff. This will be assessed by documenting sufficient supplies within the mandatory weekly report submitted to the National Healthcare Safety Network Long-Term Care module. Visitors must supply their own face mask or covering. • The facility is prepared to expand visitation and other activities for its residents, including with consideration of any special needs of its residents and other relevant safety factors. The Arkansas Department of Health will provide guidance for facilities. • The facility conducts screening of every visitor, vendor, and employee of the facility prior to entrance.
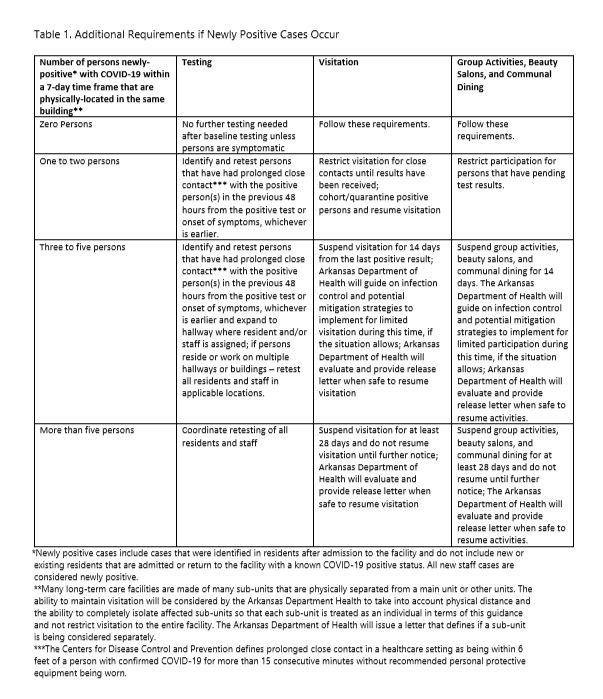
Once a facility meets these requirements, a facility may expand visitation, activities, and communal dining subject to the further requirements described below. Additional restrictions will be required if residents or staff become positive after baseline testing is complete as described in Table 1 below. Such newly positive cases include cases that were identified in residents after admission to the facility and do not include new or existing residents that are admitted or return to the facility with a known COVID-19 positive status. All new staff cases are considered newly positive.
Visitation
Visitation is recognized as an important part of a resident’s health and well-being. Reopening and progressively expanding visitation in nursing homes and assisted living facilities is encouraged once facilities satisfy the facility-specific criteria above and adhere to the standards identified. Visitation will, therefore, be allowed on a facility-specific basis when the above criteria are met. All visitation is subject to these requirements and the limitations in Table 1. The Arkansas Department of Health is available for consultation and can issue individual guidance regarding limitation of visitation for facilities in unique circumstances.
General requirements for visitation:
• Visitors must participate in and pass the facility’s screening process prior to each visit. • The facility screening process must include a screening questionnaire, which will record the identity of the resident visited, date, name, address and phone number of the visitor and maintain these records so that they can be made available upon request by the Department of Health and the Office of Longterm Care. The questionnaire will also include a declaration regarding signs and symptoms of infection, contact and/or exposure to known COVID-19 positive persons, and any prior testing for COVID-19, as well as a statement that the visitor will inform the facility immediately if they develop symptoms within 72 hours of visiting or test positive for COVID-19 after visiting. • Visitors must not have signs or symptoms of COVID-19 for at least 3 days. If any visitor previously tested positive for COVID-19, they must not visit within 14 days of a positive test. • Visitors must wear a mask at all times. • Visitors must sanitize hands with an alcohol-based hand rub or by handwashing with soap and water when entering and exiting. • Visitors cannot eat during the visit. • Visitors must schedule visits in advance. • Visitation will only be allowed during select hours of each day. • Visitation will be limited to two visitors per one resident at a time. • The facility must monitor all visits carefully to ensure that masks are worn and visitation polices are followed. • All visitors will be provided the opportunity to visit according to the number of positive cases, and the length of visits will be subject to these requirements and depend upon overall demand. • Visitation will not be allowed for residents considered to be infectious for COVID-19, which is the period of 14 days after the first positive test. The Arkansas Department of Health will provide additional guidance for visitation of residents that test positive more than 14 days after the first positive test and remain in isolation or quarantine at the facility.
Outdoor Visit Guidance
It is known that congregate settings can amplify the spread of COVID-19. However, recent data show that the risks of transmission are lower in outdoor settings. The reopening process encourages visitation to include outdoor family visitation at long-term care and assisted living facilities. Facilities should establish visitor areas that are protected from weather elements, such as porches, patios and other covered areas, or have a space that is big enough to house a temporary tent.
Requirements:
• The facility must meet general requirements for visitation, as outlined above. • The facility must monitor the temperature in any outdoor visitation areas. • Visits should occur only on days when there are no weather warnings that would put either visitors or residents at risk. • Adequate staff must be present to allow for personnel to help with the outdoor transition of residents, monitoring of visitation, and wiping down visitation areas after each visit. • The visitation area must be wiped down between visitations using an approved antiviral disinfectant. Please reference https://www.cdc.gov/coronavirus/2019-ncov/community/reopen-guidance.html. The visitation schedule will provide sufficient time in between visits for this process. • Outdoor visitation spaces must allow appropriate social distancing of at least 6 feet between visitors and loved ones. • Residents should wear a face mask during the visit, if able. • Residents must have the ability to safely transition from their room to an outdoor visitation location. • Residents with a scheduled visit who have had COVID-19 must no longer require transmission-based precautions as outlined by the CDC at the time of the visit. https://www.cdc.gov/coronavirus/2019ncov/hcp/disposition-hospitalized-patients.html. • Visitors must stay in designated outdoor visitation locations. • Visitation should be restricted to children 12 years of age or older. Visitors with children must be able to manage them, and children must be able to wear a face mask during the entire visitation. Special family circumstances warranting children under the age of 12 to visit can be approved by individual facilities. • Visitors may provide food and beverage to the resident consistent with dietary considerations, but food should not be shared between residents and visitors.
Indoor Visit Guidance
In recognition of hot weather and other uncontrollable circumstances, the reopening process includes limited indoor family visitation at long-term care and assisted living facilities. Facilities should establish visitor areas that are outside the resident’s room or private space and easily accessed without unnecessary movement within the building. Visits in a private resident room may be permitted, upon request and in the facility’s discretion, for bedbound residents or those who, for health reasons, cannot leave their room.
Requirements:
• The facility must meet general requirements for visitation, as outlined above. • Adequate staff must be present to allow for personnel to help with the transition of residents from their rooms to the visitation area, monitoring of visitation, and wiping down visitation areas after each visit. • Visitation shall be staggered throughout the day to accommodate the visitation space and appropriately limit the overall number of individuals visiting at one time. • The visitation area must be wiped down between visitations using an approved antiviral disinfectant. Please reference https://www.cdc.gov/coronavirus/2019-ncov/community/reopen-guidance.html. The visitation schedule will provide sufficient time in between visits for this process. • Visitation spaces must allow appropriate social distancing of at least 6 feet between visitors and residents.
• Residents should wear a face mask during the visit, if able. • Residents must have the ability to safely transition from their room to the visitation area, if used. • Residents who have had COVID-19 must no longer require transmission-based precautions as outlined by the CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html. • Visitors must remain in their vehicle until their scheduled visitation time. After entering the facility, visitors must stay in designated visitation locations. Visitors are not permitted to go into resident rooms without express permission granted in advance of the visit. • Visitation should be restricted to children 12 years of age or older. Visitors with children must be able to manage them, and children must be able to wear a face mask during the entire visitation. Special family circumstances warranting children under the age of 12 to visit can be approved by individual facilities. • Visitors may provide food and beverage to the resident consistent with dietary considerations, but food should not be shared between residents and visitors.
Activities
Person-centered activities are important to residents and improve resident quality of life. Progressively expanding group activities in nursing homes and assisted living facilities is encouraged when facilities satisfy the facility criteria above and adhere to the standards identified. Group activities should be allowed, on a facilityspecific basis and, subject to these requirements and the limitations in Table 1. Visitation for activities is subject to the visitation requirements and limitations described above.
• All activities must allow appropriate social distancing of at least 6 feet between residents and the individual/s leading or participating in the activity. • All residents and other participants must wear a mask. • Activities should be limited to groups of 10 or fewer individuals. • If possible, encourage doorway activities with residents wearing masks. • Residents from COVID-19, non-COVID-19, and 14-day quarantine areas should not be comingled during activities.
Beauty Salons
Beauty salon and barber services are very popular among many residents and are believed to lead to an improvement of these residents’ quality of life. Along with other activities, nursing homes and assisted living facilities can allow salons inside their facilities to reopen subject to these requirements and the limitations in Table 1. Hair salons can resume providing services to residents with the following precautions in place:
• Hairdressers, barbers, and other beauty salon staff should be screened prior to entry just like, any other visitor. • Masks must be worn by residents and beauty salon staff. • Only the beauty salon staff, nursing home staff, and a single client shall be allowed within the salon area at one time. • Appointments shall be scheduled to allow time to transport residents so that none are waiting within the salon for their service. • Appointments should be scheduled to allow proper cleaning and sanitizing of equipment between residents. • Only residents of the facility are allowed in hair salon for services; no services can be provided to outside guests. • COVID-19 positive residents and any residents who are in 14-day observation/isolation unit due to recent admit or pending test results are excluded from these services at this time.
Dining
While communal dining is important to residents’ social needs, it poses a higher risk of exposure to COVID- 19 than visitation and activities. During communal dining, it is not possible for residents to wear a mask, and there is greater air circulation that can potentially transmit the virus. Thus, we recommend implementation of modified communal dining subject to these requirements and the limitations in Table 1. If implemented, modified communal dining includes:
Requirements:
• Tables must be arranged to allow at least 6 feet between residents and 10 feet between tables. • Tables, chairs and other fixed equipment must be sanitized and wiped down following each meal service. Spray disinfectant is not recommended. Use an EPA-registered disinfectant from List N on the EPA website for surfaces. • A hand washing station or alcohol-based hand rub must be available in the dining room for use by residents and staff. • Residents who must be more closely supervised while eating shall be prioritized to use the space available. • COVID-19 positive residents and any residents who are in 14-day observation/isolation unit due to recent admit or pending test results must be excluded from communal dining at this time. • Residents shall be assigned to dine with the same 1 to 2 people. Visitors are not allowed in the dining room